Dr. Bradley has performed well over 100 facial transformations and is giving insights into the patient’s pre-and post-surgical regimens as well as how IPS® planning and guides enhance the user’s experience and result in this interview. It really was an honor for us to get this exposure into his practice.
Surgical techniques of FFS are a natural extension of my training and career in craniofacial surgery and cosmetic surgery. I love the marriage of soft and hard tissue procedures in modifying facial features. More importantly, I was drawn to this patient population. Just like any person, trans-women have the right to live their “authentic self.” FFS is an important step in having public perception match the desired gender.
My first FFS procedures were without IPS® planning. As a result, those FFS procedures took longer; I felt the outcomes could be improved.
I already had transitioned my orthognathic surgery procedures to IPS® planning with guides and custom plates. So, I was comfortable trying to plan FFS procedures with the KLS Martin engineers. Right from the beginning, I knew IPS® planning was the way to go. Along the way, we have made adjustments and improvements. With IPS® planning, one can appreciate the variations in patient anatomy and plan for that before the surgery.
We also scientifically studied IPS® planning for FFS in the bioskills lab and found it was safer, more efficient, and more accurate.
At the initial consultation, the surgeon and patient discuss how long their transition has been taking place. Before consideration of FFS, patients should be transitioning at least one year and preferably more than two years. They should also consistently be on hormonal therapy for the same amount of time. Hormone replacement therapy will have a beneficial effect on appearance, particularly with hair growth and skin/soft tissue changes. However, bony structure changes are much less likely once skeletal maturity occurs (by age 15-16 years). As for the next step, patient preference of areas for facial feature modification is discussed. In today’s era of social media platforms and online information, the patient typically has a good idea as to the features that are commonly modified during FFS. Common facial features that most patients request at initial consultation are brow recontouring and lifting, nasal reshaping, and jawline tapering. In addition, cheek augmentation, tracheal shave, and other regions may also be requested.
Subsequently, a full evaluation from top to down is performed: hairline to brow distance, degree of supraorbital and forehead projection, nasal radix location, nasal shape, intranasal and intraoral (dental) inspection, mandibular angle width and masseteric activity, chin shape, and thyroid cartilage projection in the neck.
After that, full facial images are taken along with 3D images. Vectra 3D image software morphing may be helpful in discussing rhinoplasty and genioplasty changes.
Then a 3D CT scan is ordered (1 mm cuts from apex to hyoid). The disc is obtained and sent to KLS Martin for IPS® planning.
Finally, at the pre-operative visit, the specific details of facial feature modification are discussed. At times, patients may alter the plan after consideration from the initial visit. The KLS Martin IPS® plan (guides and custom plating) and 3D images are reviewed. Procedure risks and post-operative instructions are given.
There are three different kinds of guides: the frontal sinus/supraorbital, osseous genioplasty, and mandibular angle titanium cutting guide. Let me guide you through their respective function and advantages.
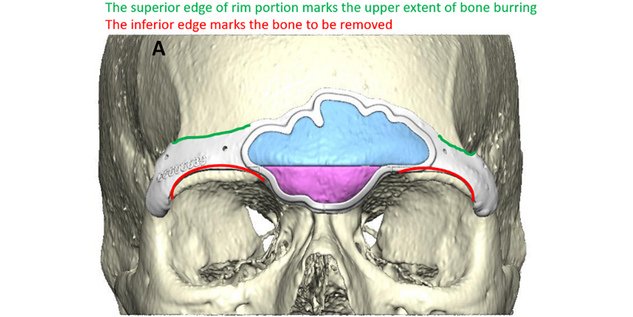
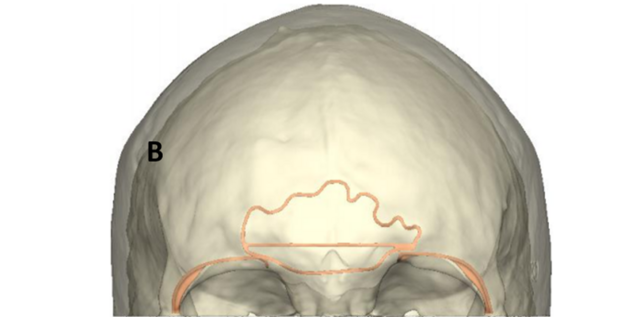
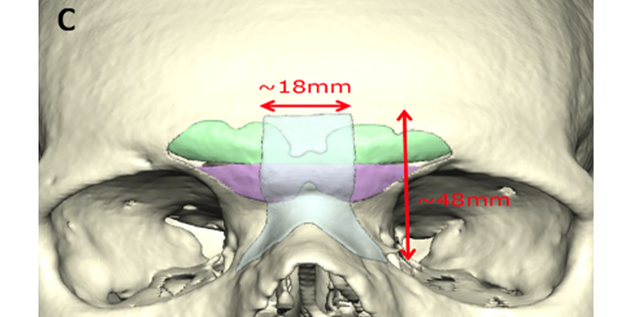
Frontal sinus/supraorbital guide: The center of this guide outlines the anterior wall of the frontal sinus. This allows for confidence in performing an osteotomy around the border of the anterior wall of the frontal sinus. There are also markings to delineate the septum of the frontal sinus. After the osteotomy of the frontal sinus wall, a thin osteotome is directed along the septal mark to complete the removal of the bone. In addition, there is a horizontal mark that delineates the most projected portion of the convex surface. This is used in making the horizontal cut across the frontal sinus once the bone has been removed. A resorbable plate is then molded (by hot water) on a pre-made clear skull model that has been modified to create a flat forehead. Frontal sinus bone pieces are secured to this resorbable plate and returned to cover the frontal sinus.
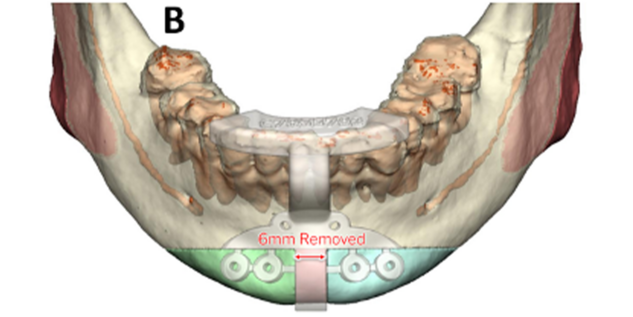
Osseous genioplasty drill and marking guide: This guide is used to mark the genioplasty horizontal osteotomy and central chin bone for removal. It also has predictive holes for the custom plate. After degloving the anterior chin, the drill and marking guide is placed based on the anterior mandibular occlusion. Screw fixation is used, and drill holes are made. A Reciprocating saw is used to cut the central bone (typically 6 mm) for removal. The horizontal osteotomy is marked as planned well below the interior alveolar/mental nerve. After down fracture, an additional thin wedge of bone angled lateral is removed for chin shortening. The patient-specific plate is then used for centralizing the two halves of genioplasty segment in an advanced position. The degree of advancement is based on surgeon preference at planning.
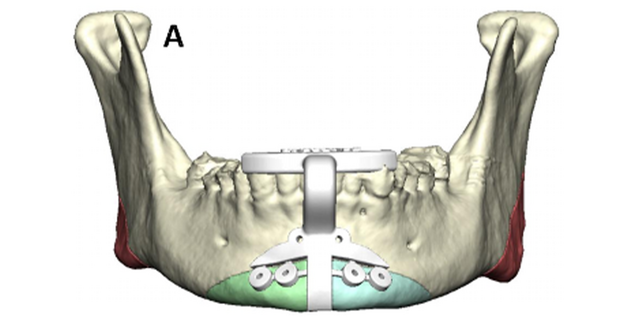
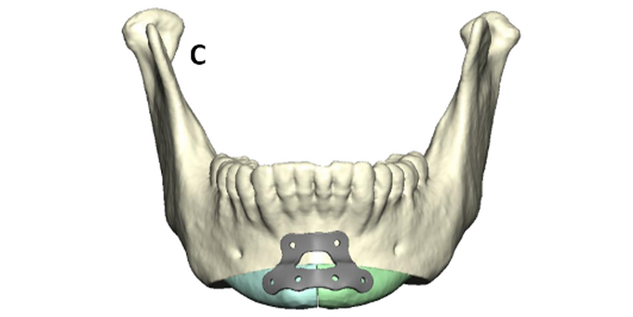
Mandibular angle titanium cutting guide: This is used to cut the mandibular angle and narrow the lower face. It is based on molar occlusion. After stripping masseteric attachments, the guide is placed and fixated to the anterior ramus with a 9 mm screw. A VRO oscillating saw is used with lighted irrigation. The saw uses the guide to “see and feel” the cut. After scoring the osteotomy, the guide is removed, and ostectomy is completed. Masseteric attachments are stripped, and bone is removed. Contour burring is performed to finalize the lateral mandibular contouring.
After FFS (performed mostly in one stage), patients typically stay in the hospital for one to two nights. After their stay in the hospital, they are asked to follow their written instruction while home and return to the office a week after FFS for their first post-operative visit. Nasal splint and sutures are removed. Swelling tends to peak in 48 hours but may take two weeks to reside. Although the profound change will be noticed almost immediately, the final result may take months.
After some time, patients adjust psychologically, which is shown in them looking forward again to wearing their makeup and styling their hair once they recover from FFS. It helps when they have friends to reach out to, that have gone through the same procedure. For other patients, we provide patient support with phone calls and texting.
If you are interested in viewing before and after images, please visit Dr. Bradley’s website: https://www.jamespbradleymd.com/
Frequently, referrals occur from within the transgender community itself. A satisfied FFS patient will often refer several friends for consultation. Local and regional transgender care facilities will refer patients directly to the office once they get positive feedback from their trans-woman clients. Internet searches and social media referrals are other common sources for referrals.
Dr. Bradley completed his plastic surgery training at NYU prior to moving to California where he completed his fellowship at UCLA under Dr. Kawamoto. Dr. Bradley spent 12 years on the West Coast prior to moving back East. He now utilizes his craniofacial training and techniques in the field of facial feminization surgery.