What do I need to take into account when planning IPS Implants® Preprosthetic?
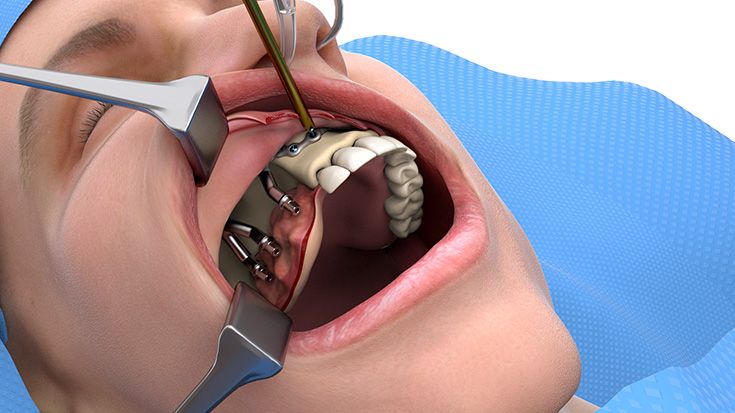
The Implant design has to be based necessarily on the following criteria:
Functionally conditions
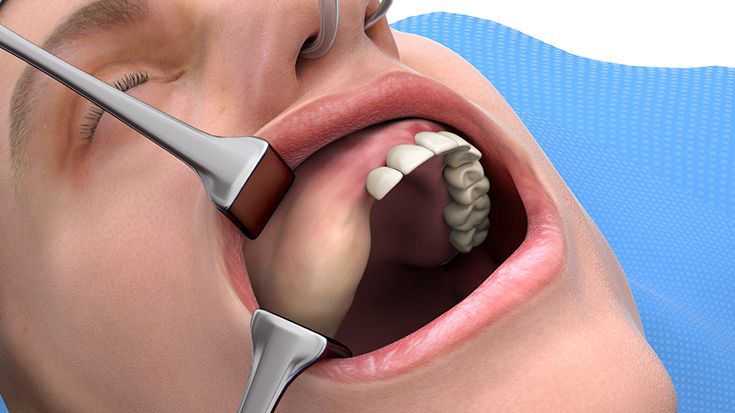
- Bite situation
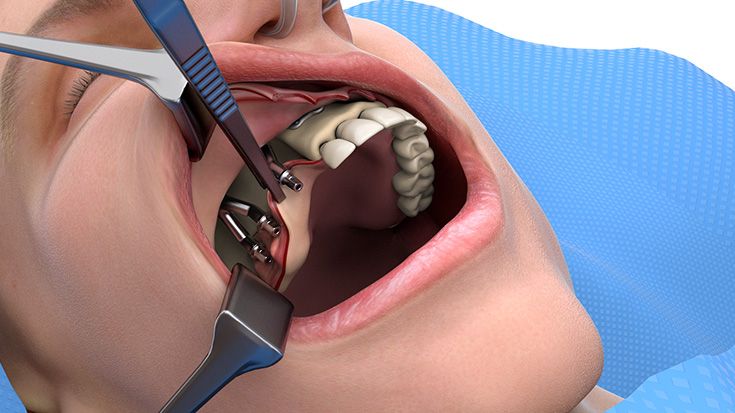
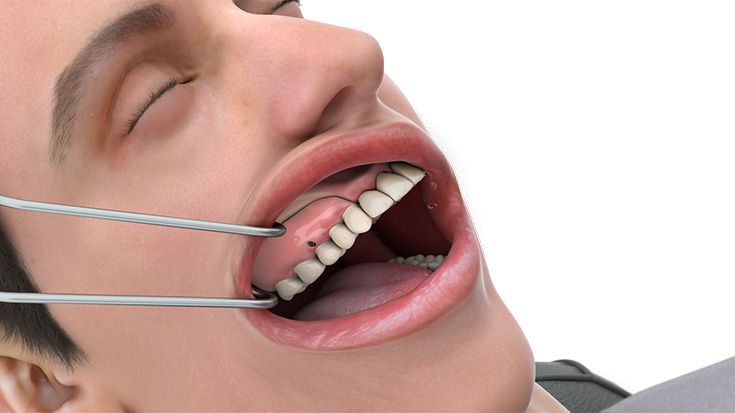
- Mouth opening
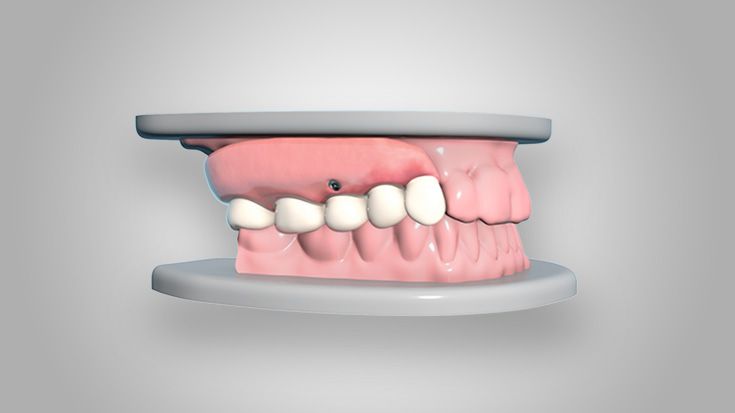
- Opposite jaw situation
- Separation of anatomical units
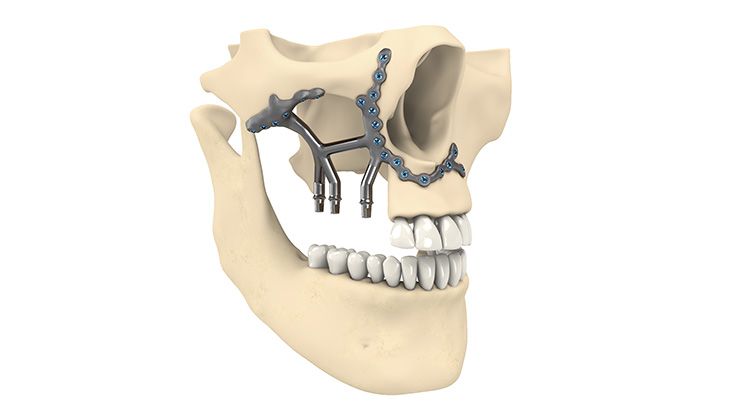
Anatomical conditions
- Soft tissue coverage and coating
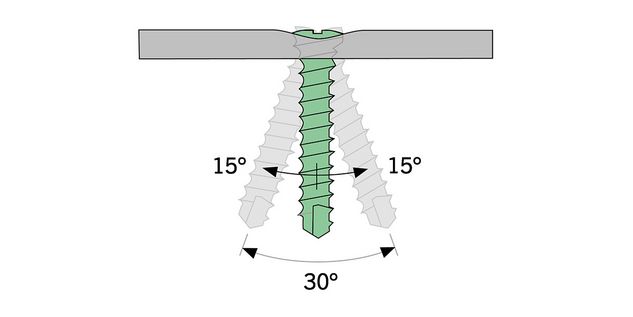
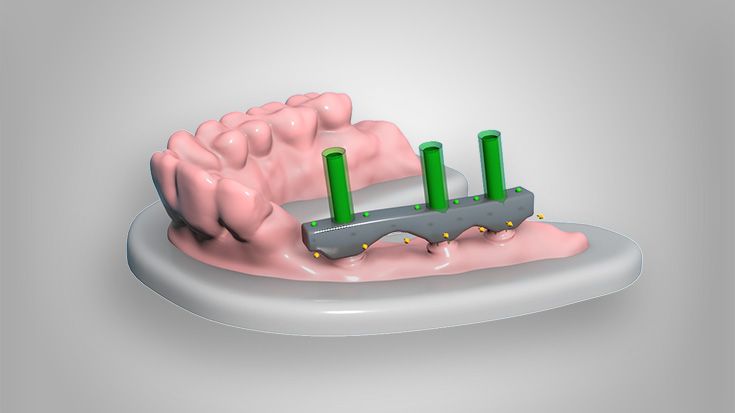
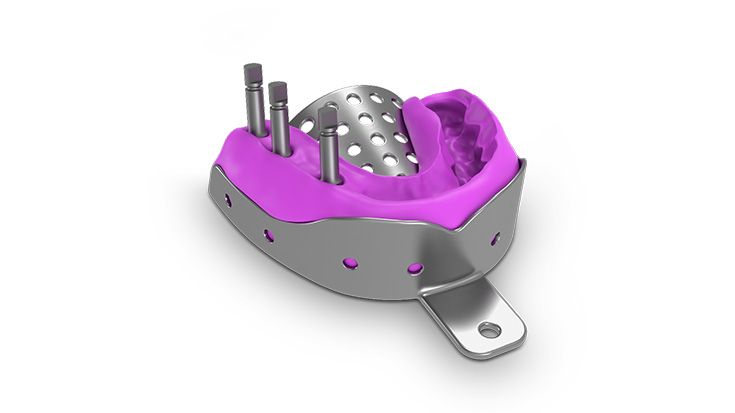
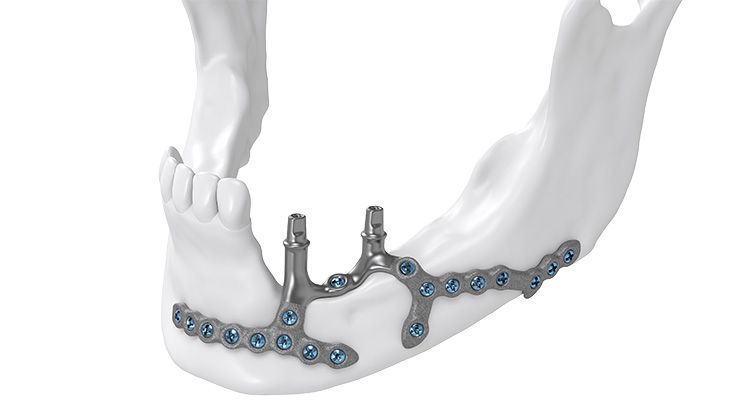
- Bone supply and anchoring possibilities
- Distance to existing metal structures like dental implants, osteosynthesis plates, mesh, etc.
Therefore, only 3D data based planning is - just like for every complex surgical prosthodontic treatment for dental rehabilitation - not sufficient alone and only one element. Furthermore the strategy for the dental rehabilitation should be rather defensive. E.g. the dentition should be planned just up to the 2nd premolar or to the 1st molar depending on the mouth opening and the soft tissue situation. For example the anatomical units in the lower oral cavity area between the cheek, vestibulum, oral cavity and tounge are not separated through an immobile and thick enough soft tissue coating so that the mobile inner cheek is confluencing with the tounge underside. In this case there has to be a soft tissue separation through tissue transplantation. But this would be also necessary for the conventional dental implant born prosthodontic treatment.
It is recommended to leave at least 6 months between the radiotherapy and the implant insertion.
In general, there should be no cemented denture manufactured onto IPS Implants® Preprosthetic. Instead, the conditional removable prosthodontic solution (e.g. bar or cone anchored) should be preferred.