What inspired you to begin performing facial feminization surgery (FFS)?
Surgical techniques of FFS are a natural extension of my training and career in craniofacial surgery and cosmetic surgery. I love the marriage of soft and hard tissue procedures in modifying facial features. More importantly, I was drawn to this patient population. Just like any person, trans-women have the right to live their “authentic self.” FFS is an important step in having public perception match the desired gender.
Can you walk us through your experience with performing FFS prior to implementing IPS® planning for these procedures and the benefits that planning now provides?
My first FFS procedures were without IPS® planning. As a result, those FFS procedures took longer; I felt the outcomes could be improved.
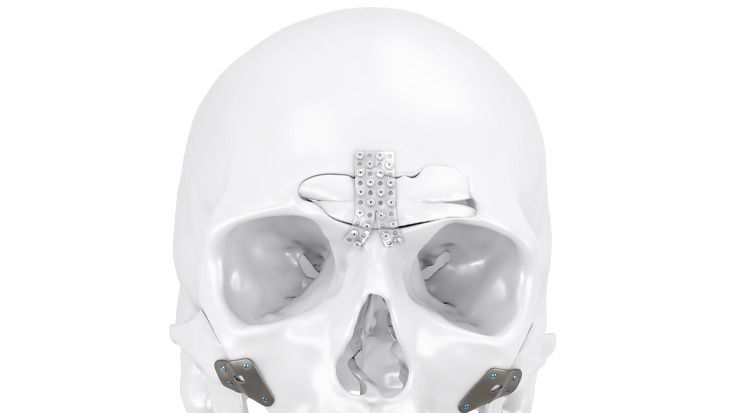
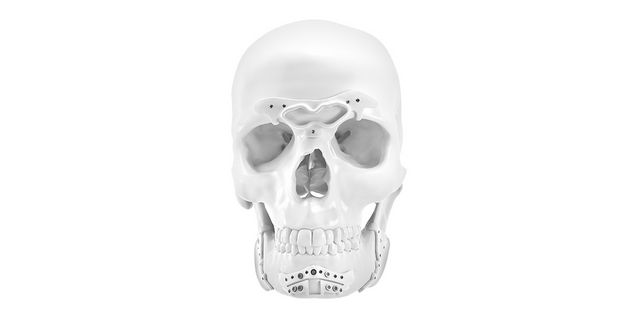
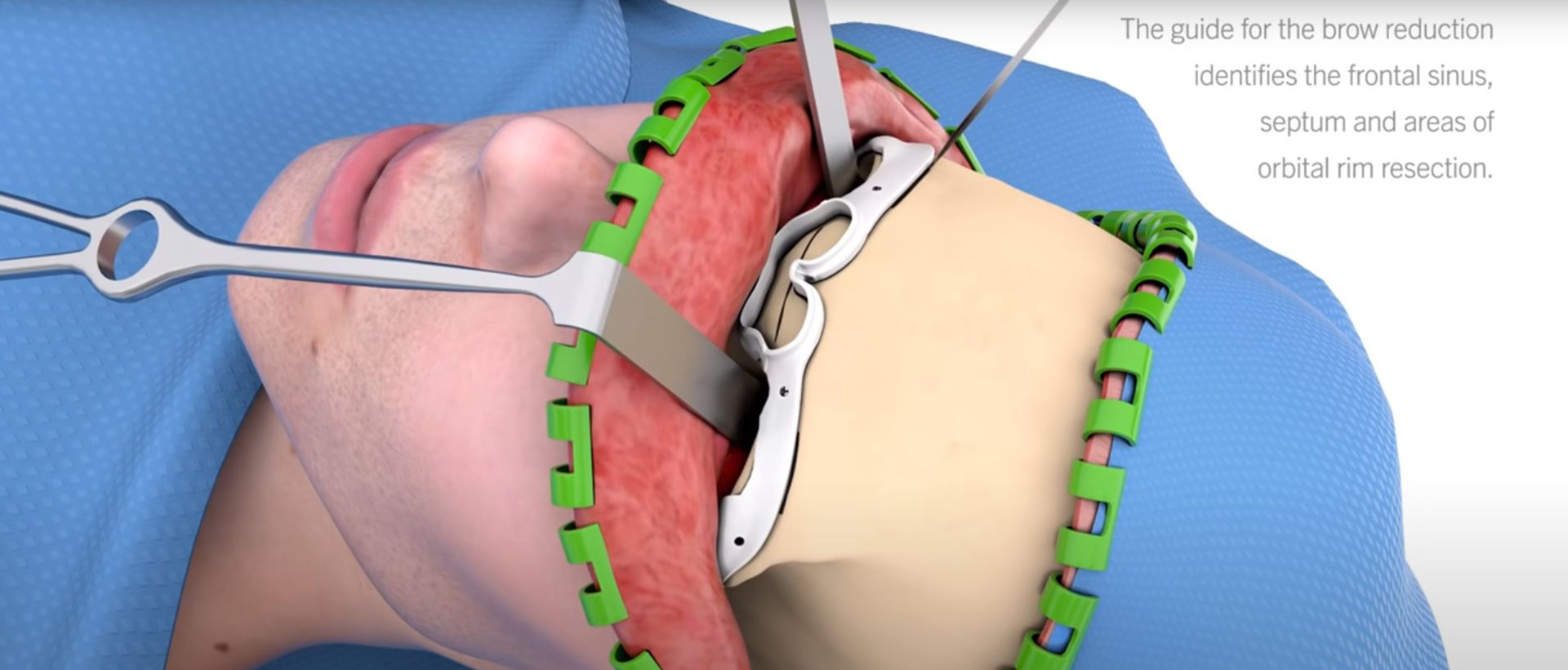
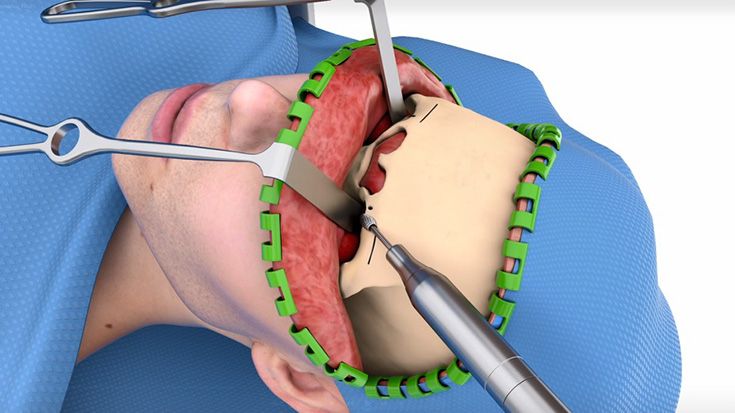
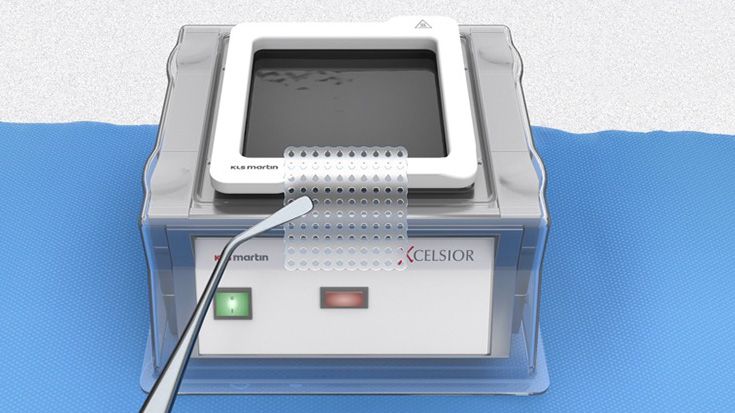
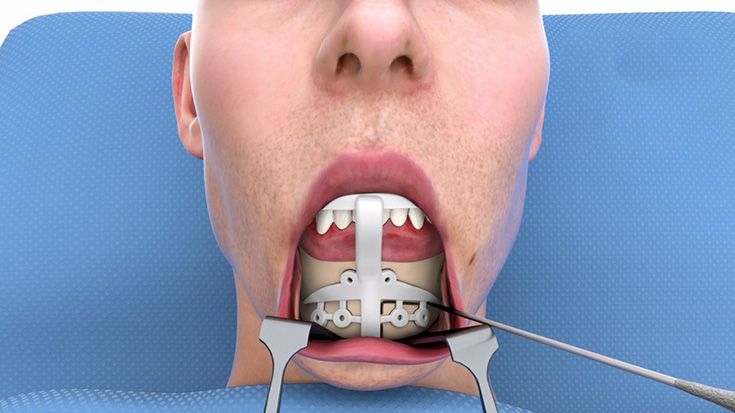
I already had transitioned my orthognathic surgery procedures to IPS® planning with guides and custom plates. So, I was comfortable trying to plan FFS procedures with the KLS Martin engineers. Right from the beginning, I knew IPS® planning was the way to go. Along the way, we have made adjustments and improvements. With IPS® planning, one can appreciate the variations in patient anatomy and plan for that before the surgery.
We also scientifically studied IPS® planning for FFS in the bioskills lab and found it was safer, more efficient, and more accurate. You can find more information to the study here.
How does the patient’s pre-surgical work look like?
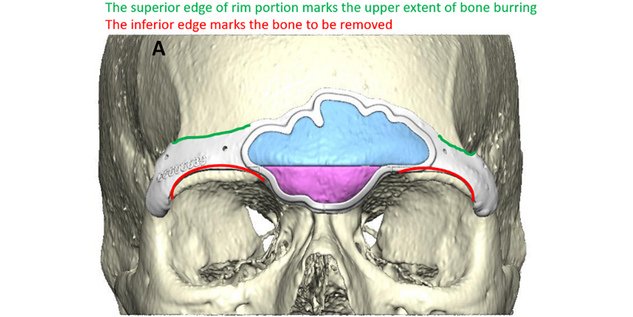
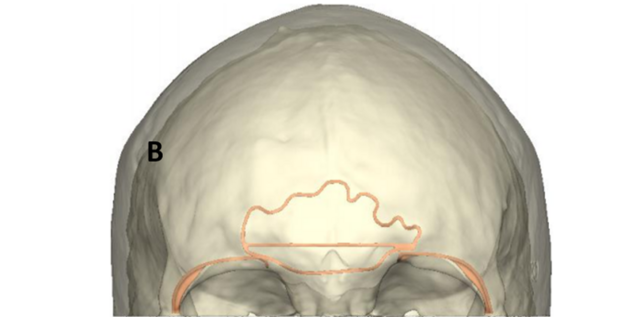
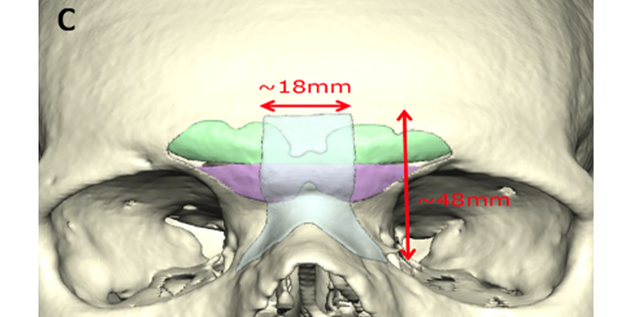
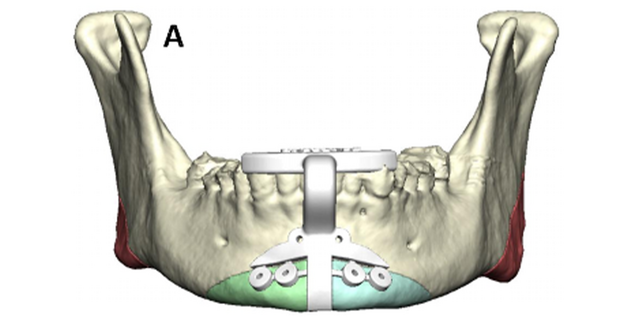
At the initial consultation, the surgeon and patient discuss how long their transition has been taking place. Before consideration of FFS, patients should be transitioning at least one year and preferably more than two years. They should also consistently be on hormonal therapy for the same amount of time. Hormone replacement therapy will have a beneficial effect on appearance, particularly with hair growth and skin/soft tissue changes. However, bony structure changes are much less likely once skeletal maturity occurs (by age 15-16 years). As for the next step, patient preference of areas for facial feature modification is discussed. In today’s era of social media platforms and online information, the patient typically has a good idea as to the features that are commonly modified during FFS. Common facial features that most patients request at initial consultation are brow recontouring and lifting, nasal reshaping, and jawline tapering. In addition, cheek augmentation, tracheal shave, and other regions may also be requested.
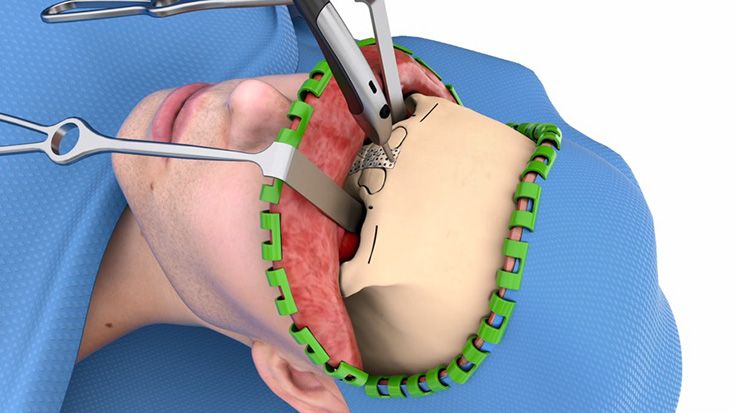
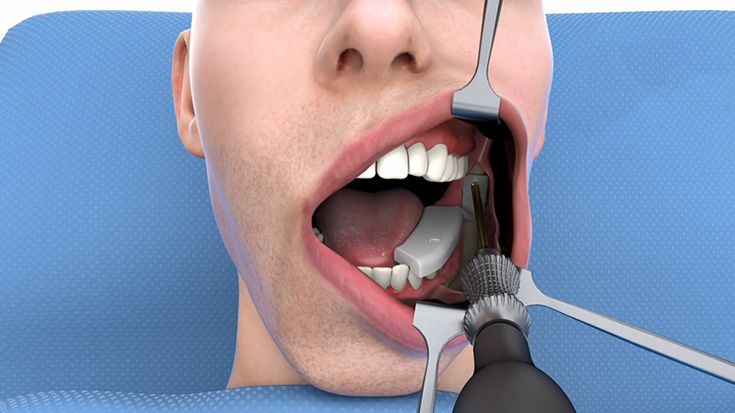
Subsequently, a full evaluation from top to down is performed: hairline to brow distance, degree of supraorbital and forehead projection, nasal radix location, nasal shape, intranasal and intraoral (dental) inspection, mandibular angle width and masseteric activity, chin shape, and thyroid cartilage projection in the neck.
After that, full facial images are taken along with 3D images. Vectra 3D image software morphing may be helpful in discussing rhinoplasty and genioplasty changes.
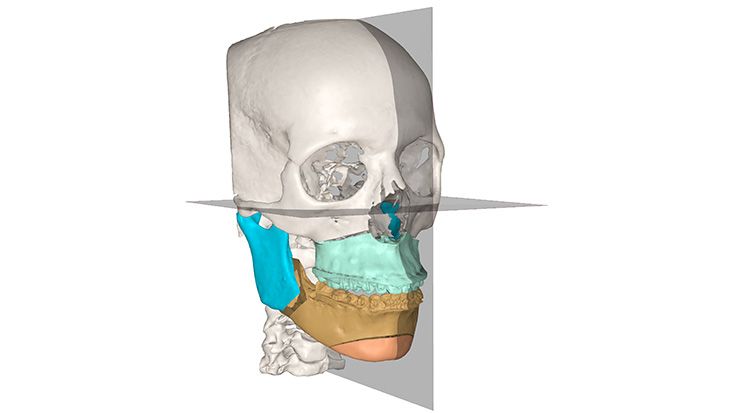
Then a 3D CT scan is ordered (1 mm cuts from apex to hyoid). The disc is obtained and sent to KLS Martin for IPS® planning.
Finally, at the pre-operative visit, the specific details of facial feature modification are discussed. At times, patients may alter the plan after consideration from the initial visit. The KLS Martin IPS® plan (guides and custom plating) and 3D images are reviewed. Procedure risks and post-operative instructions are given.
What kind of guides are used, and what are their advantages as opposed to working without one?
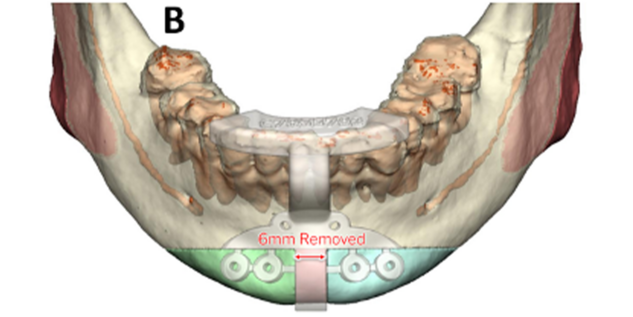
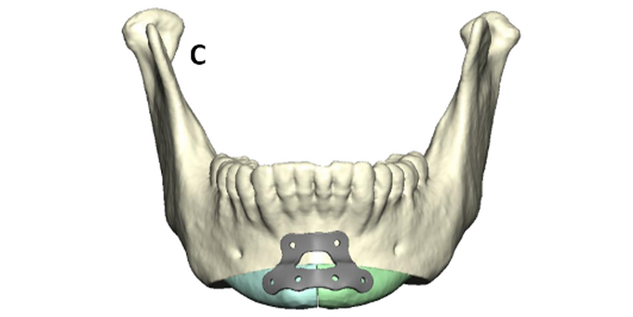
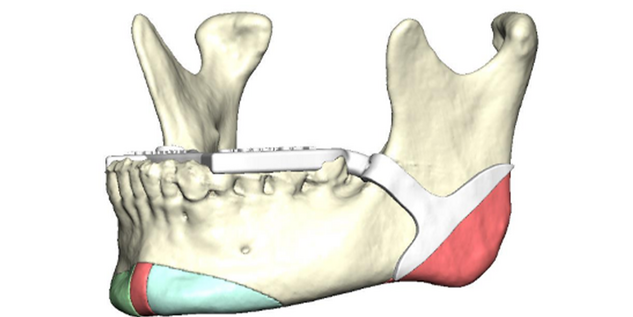
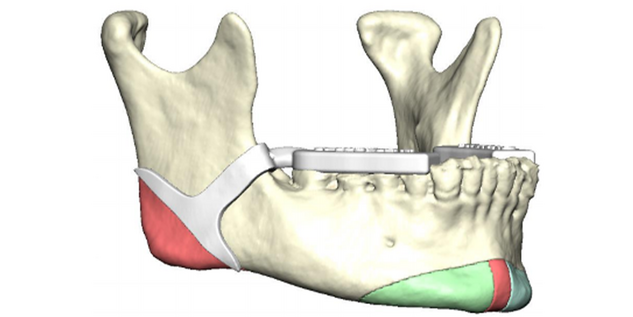
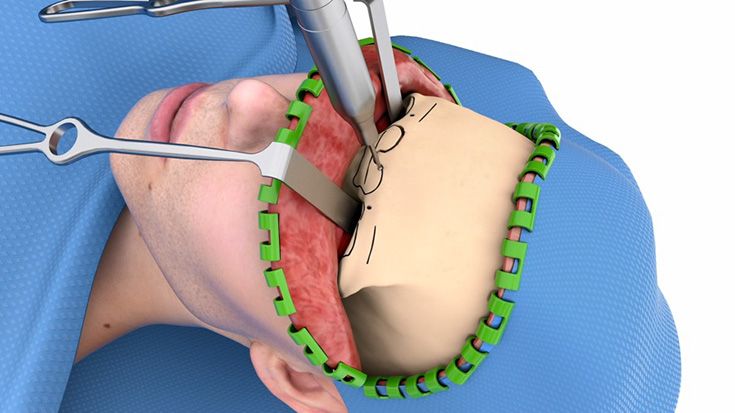
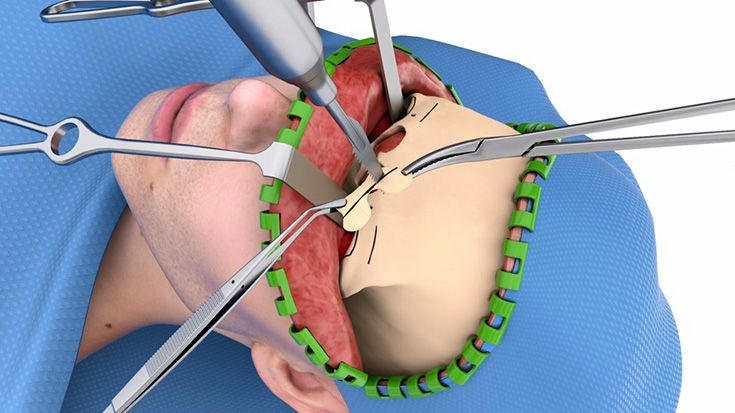
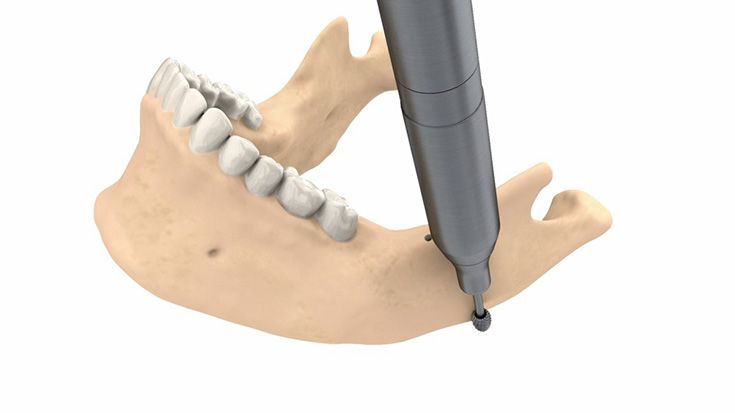
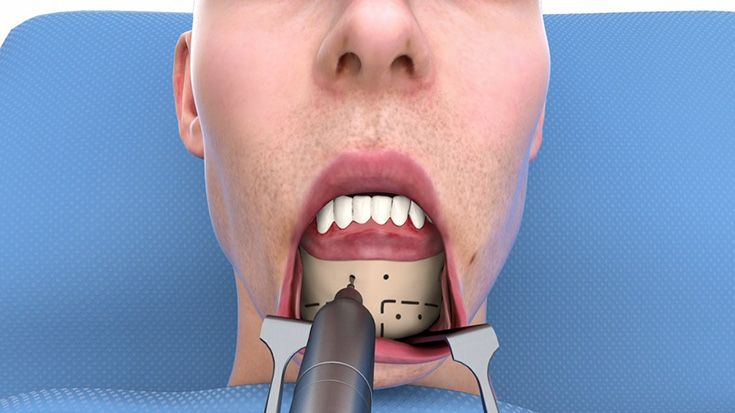
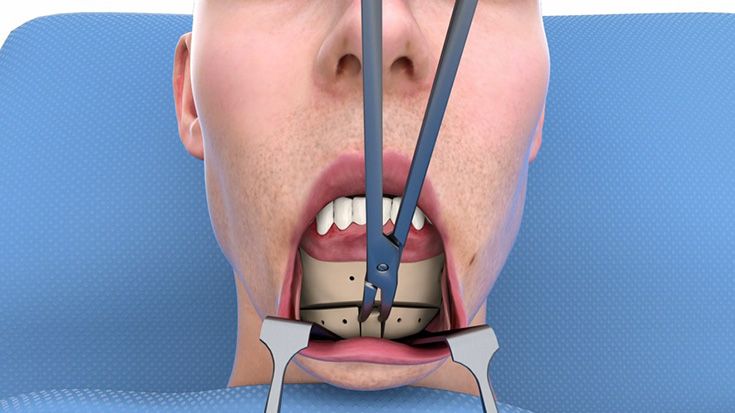
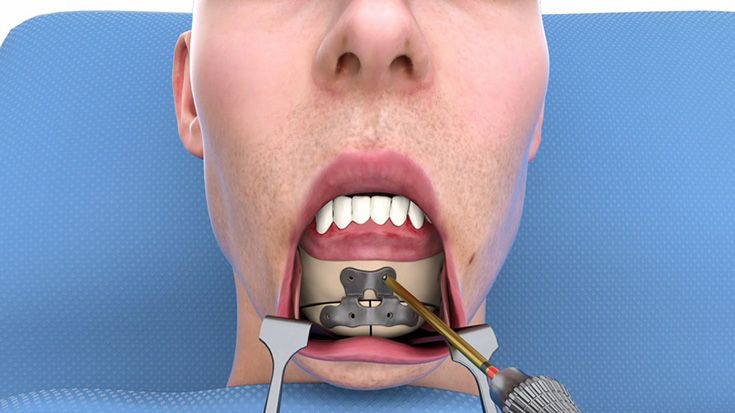
There are three different kinds of guides: the frontal sinus/supraorbital, osseous genioplasty, and mandibular angle titanium cutting guide. Let me guide you through their respective function and advantages.